Cognitive Status
Introduction
An individual's cognitive status and mental functioning is crucial information to communicate for successful care coordination at transition of care and for on-going shared care. Care coordination - when a person transitions between healthcare settings, including ambulatory care, acute care, long-term post-acute care (LTPAC), and home- and community-based services (HCBS) - is often fragmented and can lead to poor health outcomes, increased burden, and increased costs. Interoperable health information exchange has the potential to improve patient and provider communications and supports access to longitudinal health information that enables improved efficiencies, improved quality of care, and improved health outcomes. Data should be usable across the continuum of care, and beyond the traditional healthcare system - into the community.
Providers frequently are not receiving complete and accurate information including cognitive status and mental functioning in a timely manner, leading to adverse outcomes and additional expenses. Failure to exchange accurate, timely data often leads to inefficient workflows, duplicative data entries, and increased risk of patient harm attributable to missing or inaccurate information. Health Information Technology (Health IT) can significantly alleviate administrative burden by supporting health information exchange across care settings to ensure that the relevant information necessary to care for the incoming patient is delivered to the right person, at the right time- therefore improving patient outcomes, reducing provider burden, improving cost efficiencies, and improving workflows. Moreover, enhanced data exchange would allow for advanced computability, standardization, usability, and real-time data analytics, enabling broader data use by health IT developers, researchers, providers, and payers.
Poor quality discharge information is a major barrier to safe and effective transitions. With 45% of Medicare beneficiaries requiring post-acute care (PAC) services after hospitalization, the need for a seamless exchange of health information is great. The findings from a 2020 study highlight the significant gap in sharing information at transition.The survey assessed continuity between hospitals and skilled nursing facilities (SNF) and found that at transition of care complete mental status information was received by the SNF only 6% of the time. [JAMA Network Open. 2021;4(1):e2033980. doi: 10.1001/jamanetworkopen.2020.33980] .
Background
The scope of this Cognitive Status Implementation Guide (IG) focuses on exchanging cognitive and mental function observations primarily involving PAC transitions with various care settings and HCBS. While this is the start, the IG is intended to expand over time and include cognitive status and mental functioning observations not limited to post-acute care. The impetus for this initial focus is the amendment to the Social Security Act in 2014 to include the Improving Medicare Post-Acute Care Transformation (IMPACT) Act. IMPACT required the standardization and interoperability of patient assessment in specific categories for PAC settings, including long-term care hospitals (LTCHs), home health agencies (HHAs), SNFs, and inpatient rehabilitation facilities (IRFs). It focuses on standardizing data elements in specified quality measure domains and patient assessment domains for cross setting comparison and clinical information exchange, respectively.
The Act requires:
- Reporting of standardized patient assessment data through commonly used PAC assessment instruments:
- Minimum Data Set (MDS)for SNFs
- Inpatient Rehabilitation Facility - Patient Assessment Information (IRF - PAI) for IRFs
- LTCH Continuity Assessment Record and Evaluation (CARE) Data Set (LCDS) for LTCHs
- Outcome and Assessment Information Set (OASIS) for HHAs
- Implementation of data elements specified in each domain using standardized data elements to be nested within the assessment instruments currently required for submission by LTCH, IRF, SNF, and HHA providers.
- Data to be standardized and interoperable to allow exchange of data between PAC providers, among others, using common standards and definitions to provide access to longitudinal information and facilitate coordinated care.
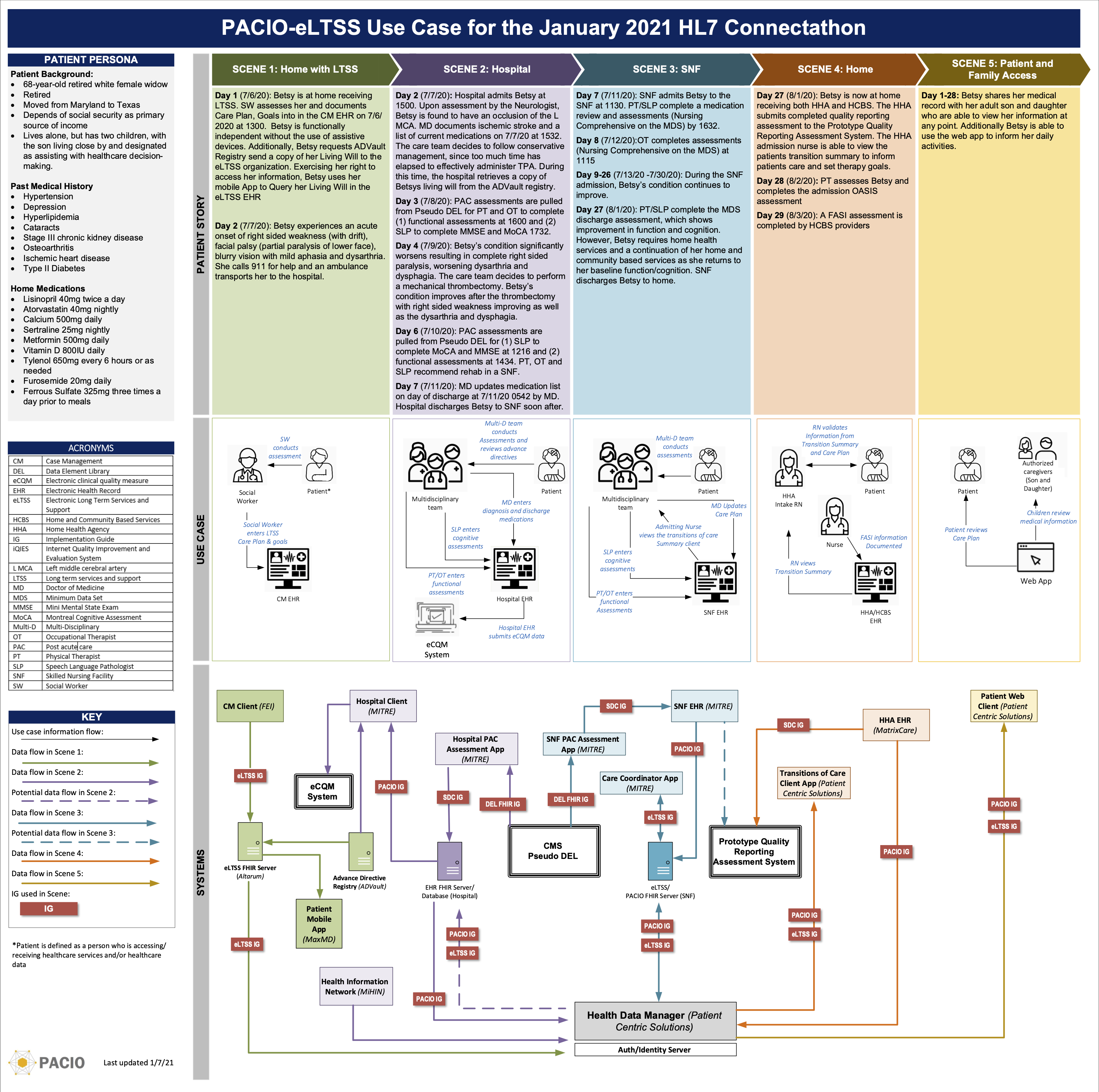
Patient Story and Data Flow Diagram