Advance Healthcare Directive Interoperability
The Advance Healthcare Directive Interoperability (ADI) FHIR implementation guide (IG) explains how to represent, exchange, and verify a person's goals, preferences and priorities for treatments and interventions regarding future medical care.
Introduction
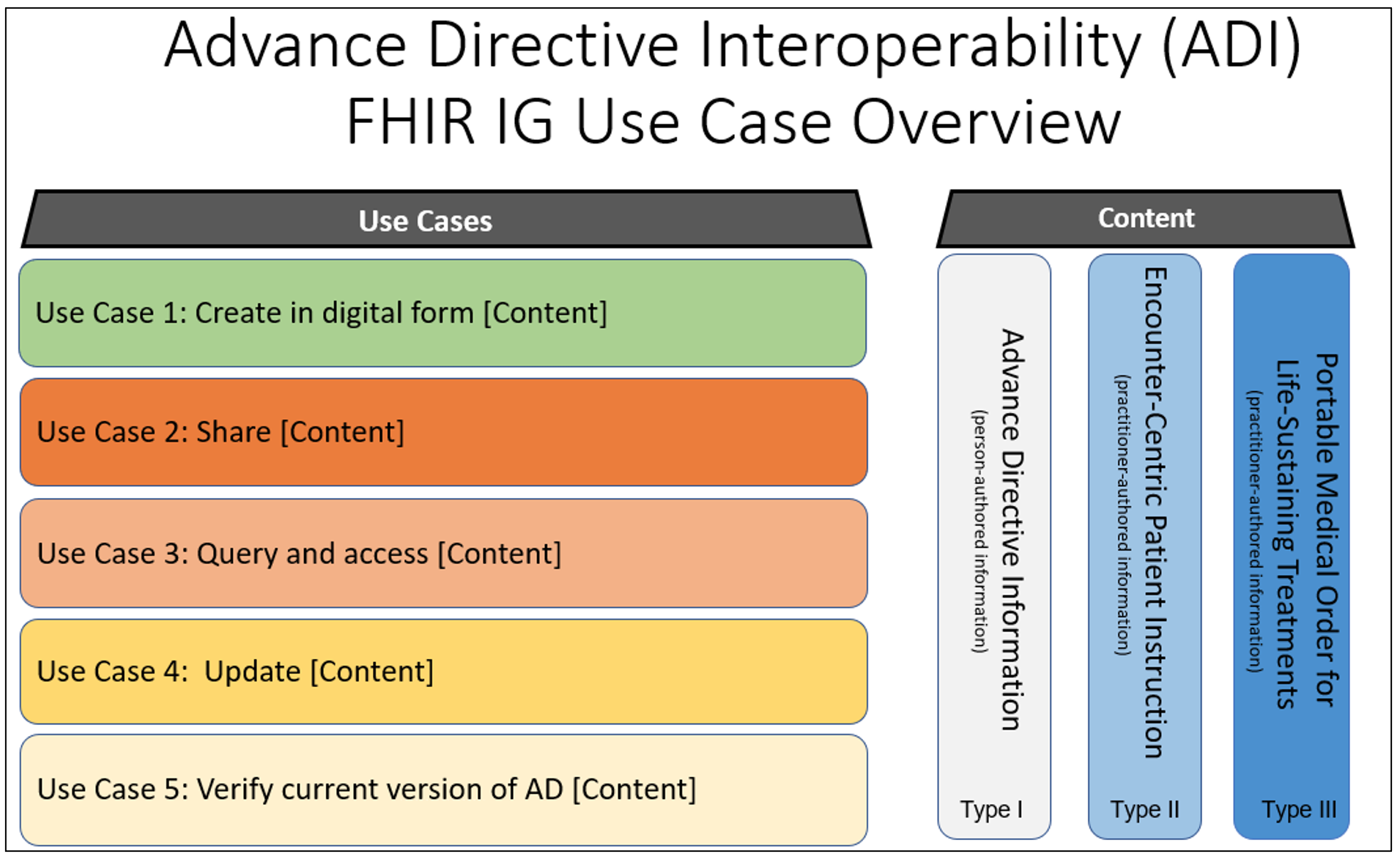
This ADI implementation guide (IG) describes how to use existing HL7 FHIR® standards to create, update, share, verify, and exchange information about an individual's advance medical goals, preferences, and priorities for care in the event the individual is unable to communicate this information to medical teams for himself or herself. Advance healthcare directives in this IG includes person-authored advance healthcare directives and personal advance care plans, and patient consent information attesting to a patient authorizing a person or persons to serve as a healthcare agent or attesting to permission granted to share advance healthcare directive information with others. It also includes practitioner-authored patient instructions (obligation and prohibitions), and practitioner-authored portable medical orders for life sustaining treatments.
Advance healthcare directives can be categorized into three types of information. The current version of this guide addresses Type I: Person-Authored Advance Healthcare Directive Information. Subsequent versions of this guide will address the other two types; Encounter-Centric Instructions and Portable Medical Order for Life-Sustaining Treatment.
Advance Healthcare Directive Overview
Background
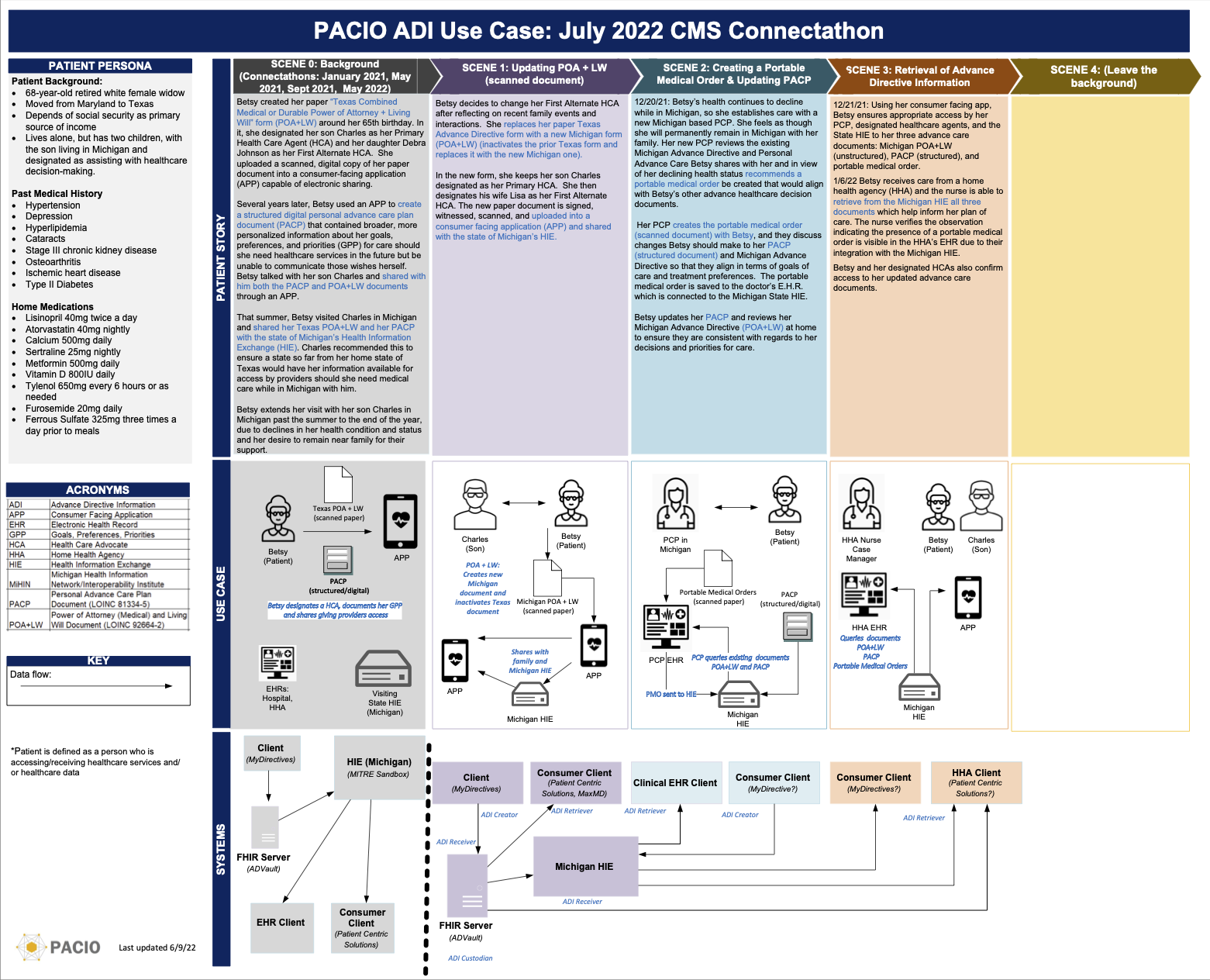
Advance healthcare directive interoperability is a complex area that involves many stakeholders. The HL7 workgroup sponsor for this FHIR IG is Patient Empowerment. HL7 co-sponsor workgroups include Patient Care, Community Based Care and Privacy, and Orders & Observations. As part of PACIO's main goal in improving care transitions, the Post-Acute Care Interoperability (PACIO) Community has adopted this project as a critical use case. The PACIO Community has a strong interest in the topic of advance healthcare directive interoperability with FHIR and will support the community engagement and technical FHIR IG development needed for advance healthcare directives interoperability. PACIO is supported by MITRE, CMS, ONC and many other stakeholders (clinical, technical, and industry associations).
FHIR profiles have been developed for several existing FHIR resources to represent advance healthcare directive content such as: living will, durable medical power of attorney, personal health goals at end of life, care experience preferences, end-of-life and emergency intervention preferences under certain circumstances, patient instructions (obligation, prohibitions, and consent), and portable medical orders for life sustaining treatments.
Patient Story and Data Flow Diagram